Introduction
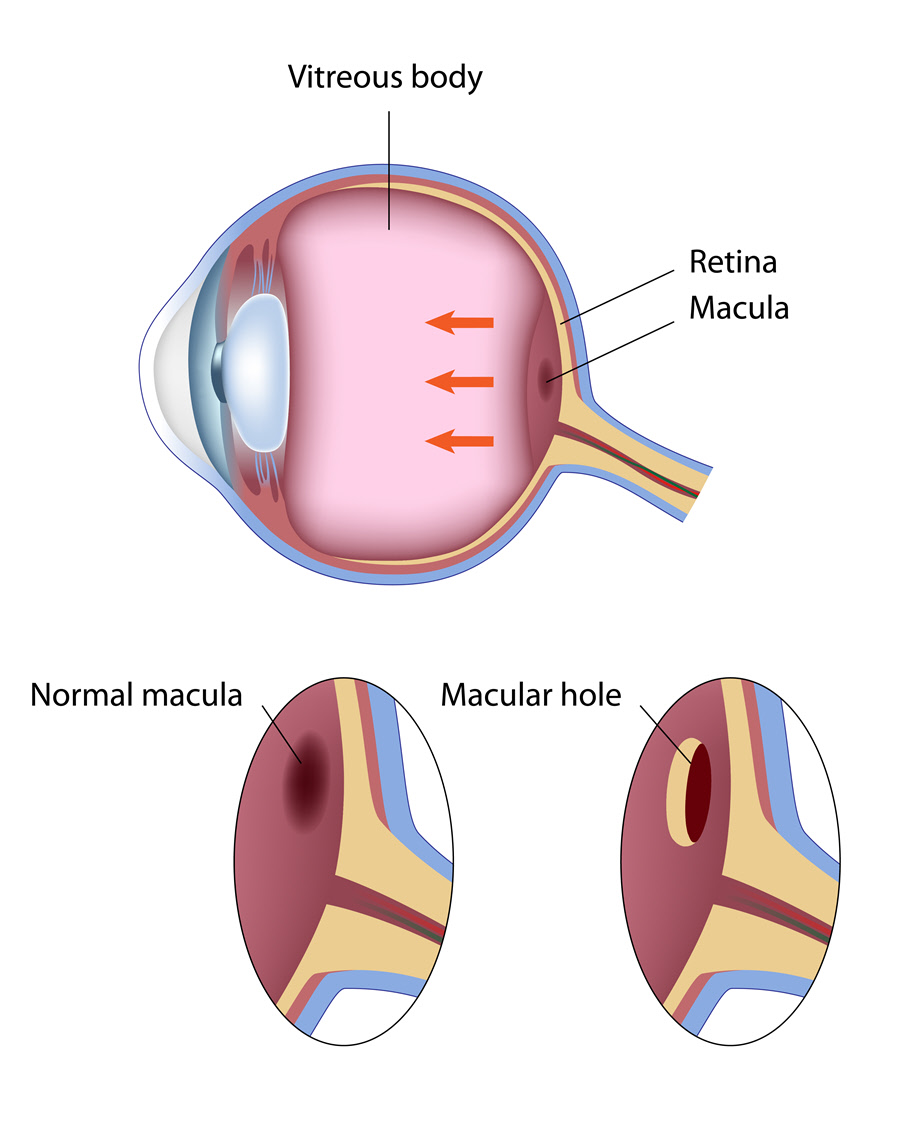
A macular hole is a tiny opening at the central part of the retina (macula). The macula is oval in shape and contains photosensitive cells referred to as cones. These cells allow for perception of fine visual details. As such, the macula plays a big role in determining visual acuity and color perception
Although the effects of the tear may be mild at the onset, a macular hole can cause massive loss of central vision.
Also Known As
- Macular cyst
- Retinal hole/tear/perforation
Sub-Types
Macular holes can be classified based on the stage of development. The stages include:
- Foveal detachment – This is the first stage where there’s loss of foveal depression. Without treatment, almost half the cases advance to the next stage.
- Partial-thickness holes – The opening tears down to the next layers of the macula in this stage. About 70% of the cases proceed to phase III if there’s no treatment.
- Full-thickness holes – This is the advanced stage. It is responsible for loss of massive central vision.
Causes and Risk Factors
As one ages, the vitreous humor begins to shrink and detach from the retina, what is referred to as vitreous detachment. This is a normal process usually causing no problems to vision. However, in instances where there is firm attachment, the pull may cause tearing. Other times, after the vitreous humor pulls away, some fibers may be left attached to the macula. Their contraction increases tension which may lead to formation of a hole. After either of the events have occurred, fluid seeps through the opening of the macula and distorts images.
A macular hole may also arise secondary to other eye conditions such as nearsightedness (myopia) or retinal detachment. Having an eye injury also increases the risk of developing a hole. The condition is said to be more common in women than men.
Signs & Symptoms
In the early stages, the patient may experience blurriness and a slight distortion in vision. With time, and if not treated, some blind spots may also appear. The macular hole, however, does not affect side vision..
Diagnosis
The diagnosis may include tests such as:
- Dilated eye exam – Dilator drops are placed in the eye for the pupil(s) to dilate. Special lens are then used to view the inside of the eye.
- Optical coherence tomography (OCT) – A machine is used to scan the back of the eye. From the imaging test, the extent of damage is determined.
- Fluorescein angiogram – This is a staining test that involves the use of fluorescein. It is useful in evaluating the condition of the macula.
Treatment
The treatment is aimed at improving vision.
Medical Treatment
Usually, the macular hole seals itself without any treatment. In a few instances, where the hole is small, the eye doctor may issue an Ocriplasmin injection to close the hole. The drug may cause some side effects which include:
- Swelling
- Light flashes
- Photophobia
- Itching and discomfort
- In severe cases, enlargement of the hole
Surgical Treatment
The most common operation performed for the treatment of a macular hole is vitrectomy. The surgery involves the removal of the vitreous gel to prevent the traction that results in tear. The vitreous gel is replaced with a gas and air bubble. The bubble holds the eye structure in place as the macular hole closes. Local anaesthesia is used during the operation to numb the eye region.
Home Care
After the surgery, the patient is required to lie or sit in a face-down position for even up to 3 weeks. This allows the bubble to lean against the opening, assisting in faster healing. The vitreous cavity refills with fluid as the bubble is reabsorbed by the eye.
After the surgery, the patient is not to travel by plane, for at least a few months. This is because the pressure can cause the bubble to expand and prevent proper healing. One should also avoid rubbing the eye. An eye patch may be worn to prevent any infections.
Prognosis/Long-term outlook
For macular holes detected early, the prognosis is favourable. After treatment, recovery can take up to three months. If not treated, patients can expect complications such as retinal detachment which requires serious intervention. Those who’ve had a macula hole in one eye are also at a high risk of developing another in the other eye.
Other complications that may arise following a macular hole are linked to surgery. After the vitrectomy, a cataract may develop, which clouds the normally clear lens. The cataract develops rapidly and will require another surgery to remove.
Prevention/Follow Up
Regular eye examinations, especially by those at risk, can help detect any problems early.