Introduction
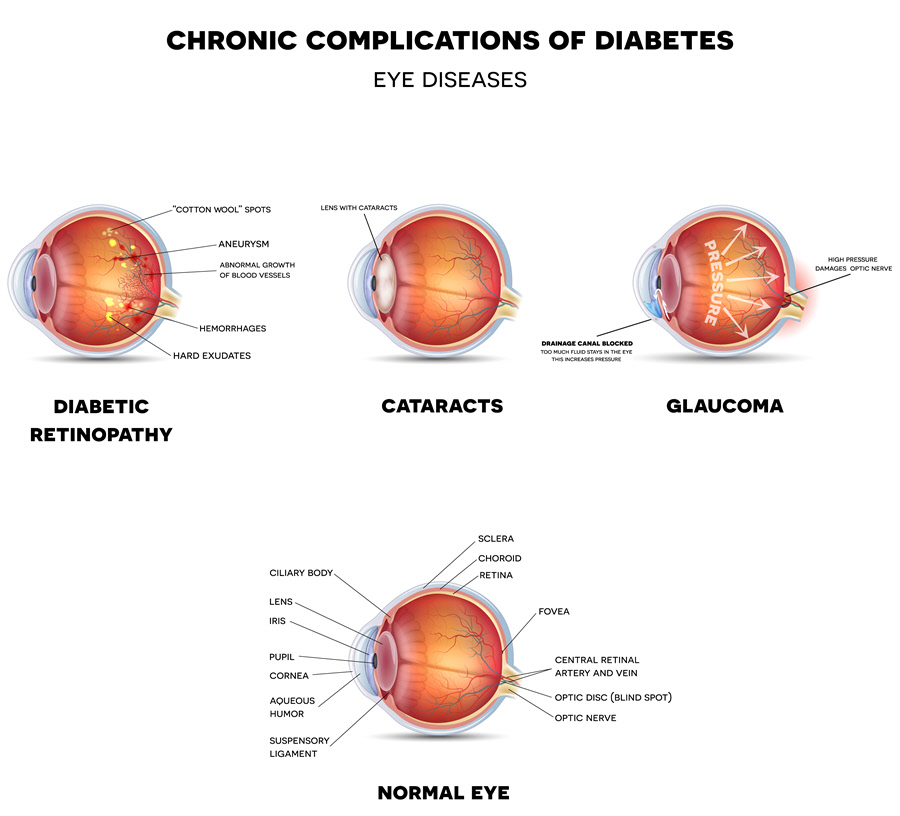
Diabetic eye disease refers to a group of eye problems that are likely to affect individuals with diabetes. The most common diseases include glaucoma, diabetic macular edema (DME), cataract and diabetic retinopathy. All eye diseases can lead to severe loss of vision and blindness due to diabetes.
Sub-Types
- Diabetic Retinopathy
Diabetic retinopathy affects the blood vessels in the retina. The retina is tissue located at the back of the eye which is also sensitive to light. In diabetic retinopathy, bleeding or leaking of fluids occurs leading to distorted vision. In the advanced stages of the disease, many new abnormal blood vessels grow on the retina’s surface resulting in scarring and the loss of cells in the retina. Diabetic retinopathy is a leading cause of blindness and vision loss to working-age adults who have diabetes. DME is the most popular cause of loss of vision among people with diabetic retinopathy. Diabetic patients, especially those who have had the condition for a long time have an increased risk of getting diabetic retinopathy.
- Diabetic Macular Edema
Diabetic macular edema results from diabetic retinopathy due to fluid that builds up in the macula. The macula is responsible for vision that enables reading, driving and recognizing faces.
- Cataract
An eye is said to have a cataract when the lens of the eye gets clouded. Vision is severely impaired necessitating eye surgery to remove the cataract.
- Glaucoma
Glaucoma may damage the optic nerve leading to blindness. The optic nerve links the eye with the brain.
Causes and Risk Factors
An individual with chronic high blood sugar from diabetes can have his/her retinal blood vessels damaged, causing diabetic retinopathy. Approximately 50% of DME patients develop diabetic retinopathy.
The leakage of fluid into the retina causes swelling in the surrounding tissue leading to DME.
Cataract is caused by the clouding of the lens mostly due to age. It usually develops at an earlier age in individuals with diabetes. The chances of an individual with diabetes developing cataracts are higher.
Glaucoma is caused by a rise in intraocular pressure (IOP) inside the eye. Diabetic adults have double the risk of getting glaucoma. People above 40 and those with a history of glaucoma in the family are also at risk.
Signs & Symptoms
Diabetic retinopathy often presents no symptoms at the beginning. Floating spots may appear. Others symptoms may include flashes, blurry vision, reduced color vision, frequently changing vision and vision loss.
DME can cause blurred vision.
Symptoms for cataracts include glare, loss of ability to discern colors, blurred vision and poor night vision.
Severe eye pain, redness in the eye, halos, headache, blurred vision, nausea and vomiting may be an indication of glaucoma.
Diagnosis
The eye care professional may detect a diabetic eye disease through a comprehensive eye examination which may include some or all of the following:
- Tonometry to check IOP
- Visual acuity testing to see how far one can see
- Pupil dilation to check the optic nerve and retina
- Optical coherence tomography (OCT) to provide detailed images of the eye
- Fluorescein angiogram to establish if the blood vessels are leaking or damaged
- A comprehensive examination to check whether the blood vessels have experienced any changes or the presence of leaky blood vessels. The exam also checks for any swellings to the macula in case of DME, damaged nerve tissue or alterations to the lens. It will measure the cornea thickness, test peripheral vision and an abnormal optic nerve in case of glaucoma.
Treatment
Medical Treatment
For DME and proliferative diabetic retinopathy (PDR), the doctor injects Anti-vascular endothelial growth factor (VEGF) medications into the vitreous gel. This injection blocks the VEGF and reverses any unusual blood vessel growth. This action decreases fluid in the retina. The drugs may also slow down progression of diabetic retinopathy. The doctor will inject or implant corticosteroids into the eye. The steroids may be used alone or combined with other drugs for the treatment of DME.
Researchers are yet to find a lasting solution for cataracts.
Eye drops or pills can treat glaucoma in its early stages.
Surgical Treatment
Vitrectomy (the surgical removal of the vitreous gel) treats diabetic retinopathy. Panretinal photocoagulation or scatter laser surgery is used to treat PDR. The laser causes the shrinking of the abnormal blood vessels.
Focal/grid macular laser surgery can be used in the treatment of DME by slowing fluid leakage and reducing the swelling in the edema.
In cataract surgery, the surgeon removes the clouded lens. He/she then exchanges it with an artificial lens.
Laser trabeculoplasty treats open-angle glaucoma by draining fluid from the eye. The surgeon can use iridotomy to create a tiny hole in the iris for people with closed-angle glaucoma to help the fluid flow to the drainage angle.
Should medications and laser surgery fail in controlling pressure, conventional surgery may correct glaucoma. The surgeon makes an opening for the fluid to flow out of the eye.
Prognosis/Long-term outlook
Corticosteroids may increase the risk of cataracts and glaucoma.
Scatter laser surgery can result in loss of night, color or side vision.
If treatment fails to improve vision, the eye doctor can recommend low vision counseling, training and other specialized services.
Prevention/Follow Up
The primary prevention of diabetic eye disease lies in controlling diabetes. Patients can do the following:
- Quit smoking
- Stay physically active
- Maintain a healthy diet
- Take medications as prescribed
- Manage diabetic ABCs which are blood sugar, blood pressure and cholesterol
- Get a comprehensive dilated eye exam annually because diabetic retinopathy can progress unnoticed
High-risk individuals can use eye drops to reduce the chance of getting glaucoma. Protection from UV radiation can help protect against cataracts.